Preemie® Visits the NICU at University Hospital Southampton, UK

On Friday 2nd June 2023, Preemie® visited the neonatal unit at the University Hospital in Southampton UK. Louise Donohue, Preemie®’s Innovation Project Manager had the privilege of visiting the Princess Anne (PA) Neonatal Intensive Care Unit (NICU) in this hospital. The UHS PA NICU is one of the UK’s leading research neonatal hospitals with special focus on preterm nutrition. The main purpose of this visit was to establish what the current process for the fortification of human milk for preterm infants currently is and how the Preemie® Sensor will integrate into the workflow and improve preterm infants’ nutritional outcomes. Prematurity is not only the leading cause of mortality in children but can also result in devastating diseases such as necrotising enterocolitis (NEC), as well as in long-term disorders and sequelae such as vision and hearing problems. Besides the tremendous impact on the quality of life of preterm infants and their families, the economic burden for the whole society is huge.
Over 6500 very preterm infants (born before 32 weeks gestation) were born in the UK in 2021. Like all infants, mother’s own milk (MOM) is the preferred feed for them. MOM has multiple health advantages including enhanced immunity and neurodevelopmental outcomes. However, preterm infants have increased nutritional requirements compared to full-term infants, and recommendations have been made by the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) regarding the optimal ranges for their nutrient intakes when fed enterally (e.g. by mouth or nasogastric tube) have been published and recently updated in 2022. MOM alone does not meet these recommendations. Therefore, maternal breast milk often requires the addition of breast milk fortifier (BMF), a commercial product specifically designed to enhance the energy, protein, mineral, and micronutrient content of breastmilk.
Currently, at the Princess Anne Neonatal Unit maternal breast milk is fortified by adding standard amounts of breast milk fortifier, which means that the NICU team provides a certain amount of the BMF per ml of MOM. These dosing recommendations are based on the assumption that all MOM is the same and provides nutrition in line with reference data for its nutrient content. However, it is well known that a mother’s milk will vary not just from day to day, but also can be different when her preterm infant is first born compared to the weeks that follow. This variability in the ‘real world’ nutrient content of MOM means that adding a standard amount of BMF does not guarantee the ESPGHAN recommendations will be met for all macronutrients (energy, carbohydrate, protein, and fat), and that the actual nutrient content of MOM with BMF added in standard amounts may often fall short of ESPGHAN recommendations. This may lead to subsequent poor growth and risk of poorer long term neurodevelopmental and cardiometabolic outcomes. Furthermore, in some cases, adding a standard amount of BMF to an amount of MOM that already has a higher nutrient content may lead to an excess of macronutrients, increasing the risk of overweight and obesity, or can result in suboptimal ratio of energy to protein, to the detriment of the infant’s growth and metabolism.
The Preemie® ecosystem enables a rapid and affordable analysis of human milk composition and delivers data-driven calculations for the targeted fortification needed to meet the unique nutritional needs of each preterm infant. The system also provides in real-time a time-stamped visualisation and analysis of the infant’s growth-related data and the corresponding nutrition given, thus supporting a retrospective understanding of fortification metrics and growth outcomes.
Preemie® has partnered with the expert team at UHS PA NICU, on a world-first ground-breaking clinical research study “Validation and clinical testing of the Preemie® Ecosystem for analysis and calculation of targeted fortification of mother’s breast milk for preterm infants”. This study is being led by Dr. Mark Johnson, the lead for NIHR Southampton Biomedical Research Centre and a neonatologist consultant specialising in preterm nutrition.
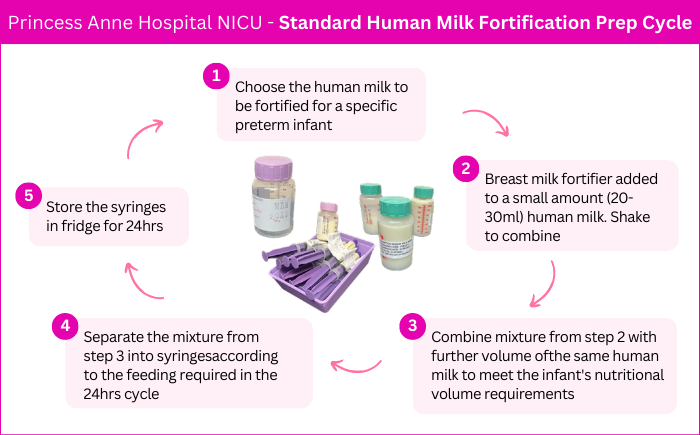
The Preemie® team, represented by Louise, met with Philippa (Pip) Crowley, Neonatal Research Nurse, Eduarda Tavares, Milk Kitchen Assistant, and Carla Smith, Milk Kitchen Assistant. In meeting the team Louise observed fully the complex operation involved with the preparation of mother’s own milk (MOM) and Donor Human Milk (DHM) for the preterm infants that they take care of in the NICU. The Preemie® team was astounded by the sheer dedication, care, and compassion the hospital team showed. Louise’s first comment while observing the Milk Kitchen team was “I am blown away by the magnitude of what goes on in this little kitchen that most people have absolutely no idea about, you have such a big and responsible job that can save the lives of these small infants”. The importance of this process is vital to ensure these preterm infants get the nutrition needed in their first few weeks of life to give them the best chance to survive and to thrive. The milk kitchen team were very generous with their time and expertise and gave the step-by-step process of the standard milk fortification and preparation they follow daily.
The nurses were equally generous with their time and expertise. Pip showed Louise around the NICU explaining the different nurseries & the vital lifesaving care given to give the preterm infants the best chance of survival. There are four nurseries in total, with 36 beds, the high-dependency nursery has 8 beds, where one-to-one nursing care is given, and astonishingly any surgeries required by the infant are performed at the bedside by the team of highly skilled surgeons. Two of the nurseries have 6 beds, and then the final nursery that all families want to get to; the 16-bed nursery where each infant will spend their last days in the NICU before being discharged home. The care is then transferred to the home team, which supports each family with the transition from hospital to home. The NICU is located on level D at the Princess Anne Hospital, UHS was not purpose-built to accommodate a NICU, it has been adapted to make use of the space available. The Preemie® team felt a real sense of the happiness and love in the unit by walking around and speaking to different members of the team (60 on each shift).
As we discussed in previous blogs, it is highly researched that mother’s own milk (MOM) is best and the team in this NICU agrees with this theory, and so encourages all mums in their care from delivery (as little as 24 weeks) to express their milk 8 times per 24 hours. If MOM is not available all infants less than 33 weeks are recommended to use Donor Human Milk (DHM), which has a better nutrient content than formula milk. UHS has a donor milk bank on site which is an excellent facility that we will feature in a future blog.
Please stay tuned for the next Blog instalment on the UHS NICU & Preemie® team visits!
The Preemie® clinical validation study project will bring together innovative human milk analysis (the Preemie® Sensor), target fortification software (NutriNTrack) to achieve individualised feeding protocols in the UHS NICU in a seamless care pathway. The goal of this project is to provide individualised targeted fortification treatment to improve the nutritional value content of the milk, be that MOM or DHM that the infant receives to enhance the overall health outcomes for each preterm patient. All preterm infants deserve the right to individualised care to meet their specific nutrition needs.



