The impact of social determinants on health outcomes in pregnant women and their infants

The power of data analysis is revolutionising all industrial sectors and the way in which many professionals work and take decisions. Healthcare makes no exception, and this is particularly true when risk prediction of developing specific conditions and diseases, as well as their management, come into play.
In neonatology, we know that several diseases are considered multi-factorial conditions, for instance Bronchopulmonary Dysplasia (BPD), meaning that many different variables contribute to their occurrence and severity. Collecting data about all such factors and monitor their changes over time can provide neonatologists with accurate risk prediction of the occurrence of the disease, and prompt preventive actions to avoid it occurs or minimise its severity.
More interestingly, data to be collected are linked to factors which do not strictly belong to the clinical sector, but can span over different categories, including demographic and socio-economic factors. A notable example is constituted by the so-called “social determinants of health” (SDoH), that is non-medical factors that influence people’s health, causing an impact in their medical outcomes, as defined by the World Health Organisation [1]. They include factors such income and social condition, education, social connections, security levels, specific habits towards health and wellbeing, such as the use of tobacco, alcohol or drugs, dietary habits and physical activity, as well as the psychological status and vulnerabilities. As we would aspect, several studies demonstrated that such factors are associated with adverse maternal effects, and above all with preterm and low birth weight births. SDoH have been identified as risk factors for preterm birth, such as low maternal socio-economic status [2], maternal medication abuse and mental stress [3], and high psychosocial vulnerability [4].
But how can such factors be tracked down and prompt interventions for reducing the health risks for the mothers and their children?
The first step is to develop a system for effective identification of the SDoH that expose mothers at higher risks for their pregnancy and for the infants. An example is the Social Vulnerability Index (SVI) developed by the Centers for Disease Control and Prevention (CDC) in the USA [5]. The index has been created to identify “at risk” communities based on the analysis of 15 different community features grouped in 4 main themes: socioeconomic status (theme 1), household composition and disability (theme 2), minority status and language (theme 3), housing type and transportation (theme 4).
Even if the SVI had been created for community interventions, a 2021 retrospective cohort study has demonstrated that the SVI is a valuable tool to identify pregnant women at high risk of preterm birth, and therefore can be used by clinicians to collect information regarding the local home environment of their patients and further refine preterm birth risk assessment [6]. The study demonstrated that mothers delivering preterm birth were more likely to live in an area with a higher overall SVI and higher vulnerability in each of the 4 themes, and that the highest SVI scores were noted among those delivering at the earliest gestational ages.
A recent study showed how the SVI can be successfully integrated into the clinical practice [7]. At first admission to the hospital, pregnant women are required to fill in the SDoH questionnaire, which includes questions related to the main themes to calculate the SVI, including financial strains, food insecurity, transport needs, physical activity, stress, social connections, housing stability, depression, use of tobacco and alcohol. As illustrated in Figure 1, the questionnaire not only generates an overall SDoH score, but generates a visual assessment of each the themes, thus providing doctors with alerts on each social determinant and detecting potential cases that need medical attention.
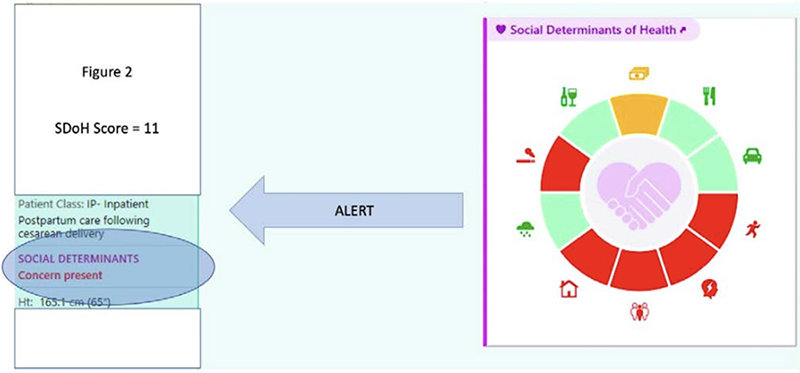
Figure 1. Screenshot of SDoH tool built-in in the electronic health records system in the hospital at the Louisiana State University
Health Sciences Center (USA). Source: Ariana Bolumen, Electronic Alerts on the Social Determinants of Health,
Neonatal Intensive Care, Vol. 35 No. 1, Winter 2022.
But how can doctors support “higher risk” women and mitigate the impact of social determinants on the health outcomes of mothers and of their infants?
Another recent study aims to provide an effective answer [4]. The study intends to determine the effectiveness of preventive interventions to reduce preterm birth among pregnant women with psychosocial vulnerability factors, through a systematic review of preventive interventions. As a result of the analysis, massages provided by partners and group meetings showed to have a significant preventive effect on preterm birth, while other interventions such as home visits and phone calls had no significant preventive effect. Furthermore, the use of financial income supplement showed a reduction in preterm births. Besides the effectiveness of single interventions, which is questioned since the studies reviewed have moderate or high risk of bias, two conclusions seem to be particularly important.
The first is that pregnant women with different vulnerabilities are often offered the same intervention, although research shows that interventions should be tailored to each woman’s needs and circumstances. This shows that also the social determinants of health need a person-centric, tailored approach in order to minimise their adverse impact on pregnant women and on their infants.
The second is that the level of evidence for such kind of interventions is still very limited, and lacks quality research with robust designs and sample sizes providing recommendation of specific programmes to reduce preterm birth among vulnerable pregnant women. In this case, we firmly believe that the power of data analysis and the use of innovative techniques such as Artificial Intelligence and Machine Learning can provide unique insights into the weight that each risk factor has on preterm birth, as well as into the most effective interventions tailored for the unique vulnerabilities that pregnant women experience.
Innovative approaches based on AI-backed data analysis can boost game-changing approaches, facilitate the evaluation of the effectiveness of personalised approaches, and guide policies and clinical practice to take in consideration socio-economic determinants of health and effectively prevent their impact on health outcomes.
Bibliography
[1] https://www.who.int/health-topics/social-determinants-of-health
[2] Amjad S, MacDonald I, Chambers T, et al. Social determinants of health and adverse maternal and birth outcomes in adolescent pregnancies: A systematic review and meta- analysis. Paediatr Perinat Epidemiol. 2019;33(1):88-99. doi:10.1111/ppe.12529
[3] Moradi G, Zokaeii M, Goodarzi E, Khazaei Z. Maternal risk factors for low birth weight infants: A nested case-control study of rural areas in Kurdistan (western of Iran). J Prev Med Hyg. 2021;62(2):E399-E406. Published 2021 Jul 30. doi:10.15167/2421-4248/jpmh2021.62.2.1635
[4] Pedersen JF, Kallesøe SB, Langergaard S, Overgaard C. Interventions to reduce preterm birth in pregnant women with psychosocial vulnerability factors-A systematic review. Midwifery. 2021;100:103018. doi:10.1016/j. midw.2021.103018
[5] https://www.atsdr.cdc.gov/placeandhealth/svi/index.html
[6] Givens M, Teal EN, Patel V, Manuck TA. Preterm birth among pregnant women living in areas with high social vulnerability. Am J Obstet Gynecol MFM. 2021;3(5):100414. doi:10.1016/j.ajogmf.2021.100414
[7] Ariana Bolumen, Electronic Alerts on the Social Determinants of Health, Neonatal Intensive Care, Vol. 35 No. 1, Winter 2022.

