6th International Congress of the European Milk Bank Association

On October 15th – 16th 2021, the Preemie system attended and supported the latest 2021 EMBA International Congress, which took place in Warsaw. The 2021 EMBA International Congress, one of the most prestigious events in the field, reunited the most reputable researchers in neonatology and infants’ nutrition from all over the world.
This year’s event was organized as a hybrid congress, which made it possible for the attendees to attend the event in person or using a dedicated digital platform.
The Preemie system was represented by our COO Paolo Satta, who presented the latest “Cost-Benefit Analysis comparing Targeted Fortification Versus Standard Fortification Approach for Very Low Birth Weight Infants”. The 15-minute presentation was aimed at answering a key question: “Is targeted fortification cost-beneficial?”.
By considering a 50-bed Neonatal Intensive Care Unit (NICU) performing human milk analyses every day as a reference scenario, the study started presenting the overall costs to be borne in order to adopt targeted fortification. The costs for using different human milk analyzers had been identified, encompassing the purchase of the analyzer and other equipment, costs for consumables, the increased labour costs for both performing human milk analysis and calculating the fortification needed, and also the costs for wasted milk. Expected cumulative costs after 10 years of usage range in between $565,000 and $1,060,000.
The following step was to present the potential benefits, by referencing to relevant literature for what concerns the expected health outcomes, that is the reduction in the prevalence of key disease: necrotising enterocolitis (NEC), bronchopulmonary dysplasia (BPD), and sepsis. By considering the percentage of reduction reported in various studies and the incremental costs associated with the occurrence of the identified diseases, the potential economic savings associated to disease reduction were presented. Annual savings can be huge, ranging from almost $650,000 just for NEC reduction, to almost $400,000 for sepsis reduction, and $500,000 for BPD reduction. If such health outcomes are confirmed by larger clinical trials (and possibly other outcomes are identified), the savings in just 1 year of targeted fortification would cover the costs for 10-year usage of the targeted fortification approach.
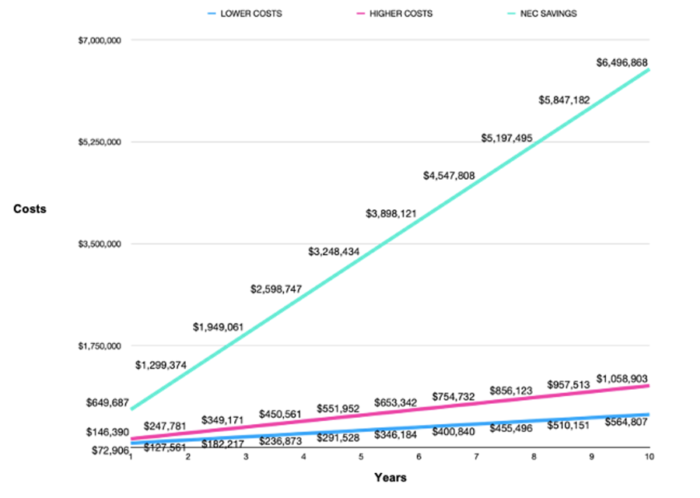
Figure 1. Savings expected just for NEC reduction entirely cover the costs for targeted fortification, and in less than 2 years pay back the expenses for 10-year adoption of the approach.
The presentation ended with a final question: in case that only one health outcome (for instance NEC reduction) is confirmed and not the others, what is the reduction rate needed to cover the costs of the targeted fortification approach? The results are surprisingly very low. Let’s take just the NEC use case: a net reduction in the order of 0.34-0.65% in NEC prevalence would cover the targeted fortification costs, corresponding to 11 to 21 NEC cases avoided in 10 years in the 50-bed NICU unit. Studies available to date report much higher net reduction rates, up to 4% for NEC.
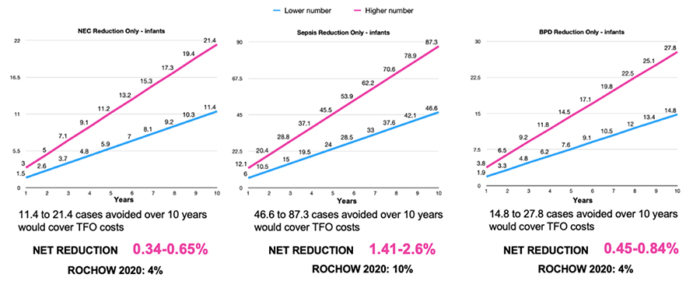
Figure 2. A very reasonable reduction in each disease’s prevalence rate would cover the costs of the targeted fortification approach. Such reduction rate is quite lower than the one reported in literature.
This allowed the presentation to reach this conclusion: we certainly need more studies on targeted fortification, larger clinical trials with limited biases and large infants’ groups, but the result of this preliminary analysis is that “targeted fortification is very, very likely cost-beneficial”.
As a final call to action, the audience was invited to interact with Preemie to perform use-case studies based on actual data from the NICU. Preemie designed a Cost-Benefit Analysis Model which can be filled in with the actual data of the NICU (for instance, number of infants hospitalized, number of infants with diseases, costs for adopting a targeted fortification approach, actual reduction of diseases, etc.), predict the expected savings when adopting the targeted fortification approach, and then track data over time to confirm the extent of the savings. This CBA Model could become a reference tool for administrators to track expenses and savings linked to infants’ nutrition, and we are eager to collaborate with NICUs to streamline our approach.
Therefore, don’t miss the opportunity to collaborate with us and reach out by writing at info@preemiesensor.com.
Feel free to read more about the CBA study here.

